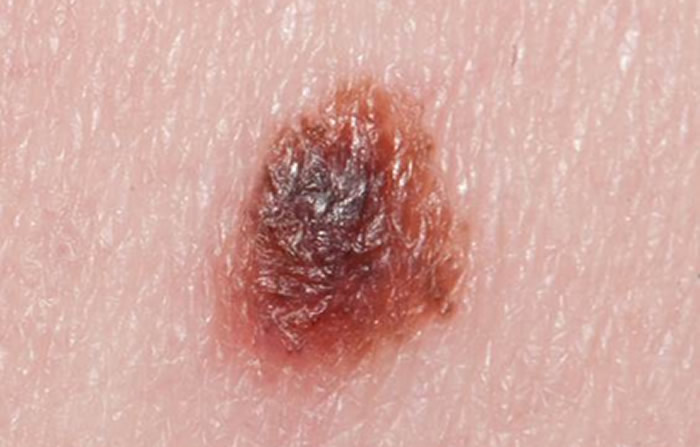
Melanoma

What is melanoma?
Melanoma is a serious type of skin cancer, arising from the colour producing cells (melanocytes) in the skin. In a melanoma, these melanocytes become malignant and grow excessively. Exposure to excess ultraviolet light from the sun is one of the most important causes of melanoma. The use of sunbeds also greatly increases the risk of getting a melanoma.
Melanocytes produce a pigment called melanin. The first sign of a possible melanoma developing is a previous mole changing in colour or a new freckle developing on the skin.
Melanoma is considered the most serious type of skin cancer because it is more likely to spread (metastasise) from the skin to other parts of the body than other types of skin cancer. There are 2000 deaths per year in the UK from melanoma. It is therefore crucial that any mole on your skin is assessed at the earliest opportunity by an expert Consultant Dermatologist like Dr Hussain who specialises in the diagnosis and management of skin cancer.
How is melanoma diagnosed?
Although a diagnosis of melanoma is serious, if caught at an early stage, most melanomas do not cause on going problems. The thinner the melanoma is in the skin at the time of diagnosis, the greater the chance of cure. If the diagnosis of melanoma is delayed, this gives the melanoma more chance to establish deeper roots in the skin. There is then a higher risk of the melanoma spreading, which can reduce life expectancy.
The most important treatment for a suspected melanoma is to cut out all of the melanoma cells with a narrow safety margin, under local anaesthetic. . The specimen that is removed from the skin is then examined under a microscope for two main reasons. Firstly, to see whether the suspicious mole was in fact a melanoma. And secondly to see if it has been fully removed and if so, how deep any roots are in the skin. This is the only way a diagnosis of melanoma can be confirmed with certainty.
Staging of melanoma
Staging systems for melanoma indicate the prognosis (outlook) from the melanoma and also the best treatments that should be employed. In the UK melanoma is staged from 1 to 4.
Stage 1 is an early (thin) melanoma and stage 4 is the most advanced, thick melanoma. The staging system takes into account if there has been any spread of melanoma from the skin to other parts of the body. Stage 1 & 2 melanomas are present in the skin only and have not spread elsewhere in the body. Stage 3 and 4 melanomas have spread to other parts of the body (metastasised).


Certain features of the melanoma will be assessed by the pathologist under the microscope when the melanoma is removed. The most important of these features is called the Breslow thickness, which measures how far the roots of the melanoma have grown down into the layers of skin. There are other features that will also be assessed by the pathologist for example if blood vessels or lymph glands are involved and how well behaving the individual melanoma cells are.
What happens after the diagnosis of melanoma is made?
Dr Hussain is Chair of the Specialist Skin Cancer Multi-disciplinary team. This comprises a group of experts (including dermatologists, plastic surgeons, pathologists, oncologists and specialist nurses) who may meet to discuss the best treatment option(s) for you. Dr Hussain prides himself in explaining things to you in terms you can understand, without the medical jargon that can often confuse many patients. Dr Hussain will take all the time you need to explain your diagnosis to you and the best way of treating your melanoma.
How is melanoma treated?
Once the melanoma has been surgically removed by Dr Hussain, this offers you the best chance of a complete cure. Indeed, in thin, stage 1 melanoma, surgical removal is all that is needed. Most patients do NOT need radiotherapy or chemotherapy.
After Dr Hussain has removed the melanoma to be accurately categorised under the microscope & has seen the report, he will then discuss a second surgical procedure to minimise the chances of a local recurrence ie to minimise the melanoma causing you any problems in the future. This second surgical procedure (called a wide local excision) is also performed under local anaesthetic & involves removing a further margin of skin around & beneath the original scar site. Dr Hussain will discuss with you in great detail if this is what you need.
What is the scar like following a wide local excision of a melanoma?
Dr Hussain will discuss with you in great detail the surgical technique that will be required for your wide local excision. To minimise the tension on the wound and in an attempt to provide you with the best long term cosmetic result, Dr Hussain often undertakes flap reconstruction following a wide local excision but this will vary according to where the surgery is taking place and individual patient factors such as the mobility & quality of your skin.
How often will Dr Hussain see me after treating the melanoma?
Dr Hussain likes to keep a close eye on all his patients after surgery to ensure everything is healing according to plan & that you have no undue concerns that haven’t been addressed. To ensure the melanoma hasn’t come back, Dr Hussain will keep you under review between one to five years after your surgery. For the first two years, follow-up appointments are every three months. After this time, assuming all is well you will be seen every six months.
During these follow-up visits Dr Hussain will examine the area of the melanoma scar and also check your lymph nodes (glands) and feel your abdomen. Dr Hussain will also carefully assess your skin to ensure there are no signs of any new melanomas having developed.
Dr Hussain may ask your GP to refer you for clinical photography to help you monitor your skin & compare the way your moles look now with how they looked before.
The most important message that Dr Hussain gives regarding any unusual or changing mole on the skin is: ‘If in doubt…..check it out’!!!
If you have any questions or comments, or if you want to learn more about the services of Dr Walayat Hussain, please call 0113 388 2234 or submit an online form by clicking here.

